In-hospital cardiac arrests (CODE BLUE) occur in both large and small healthcare facilities, and the outcomes are usually quite disappointing. The percentage of the 200,000 patients who experience in-hospital cardiac arrest every year in the United States and survive to discharge is surprisingly low [only 17% – 20% according to the Society of Hospital Medicine¹]. This may not be surprising given that patients who experience in-hospital cardiac arrest are often fragile with medical conditions that include underlying cardiac disease and multiple co-morbidities that complicate their cardiac status.
Improving the care for Code Blue patients is a complex and multifaceted issue. When a patient experiences a cardiac arrest, the need for immediate high-quality care directed by published guidelines, grounded in high-quality science, is obvious. Equally important is the capture of the care that is provided to cardiac arrest patients. Ensuring that the event is well documented and that the documentation is immediately available for post-arrest patient care is essential.
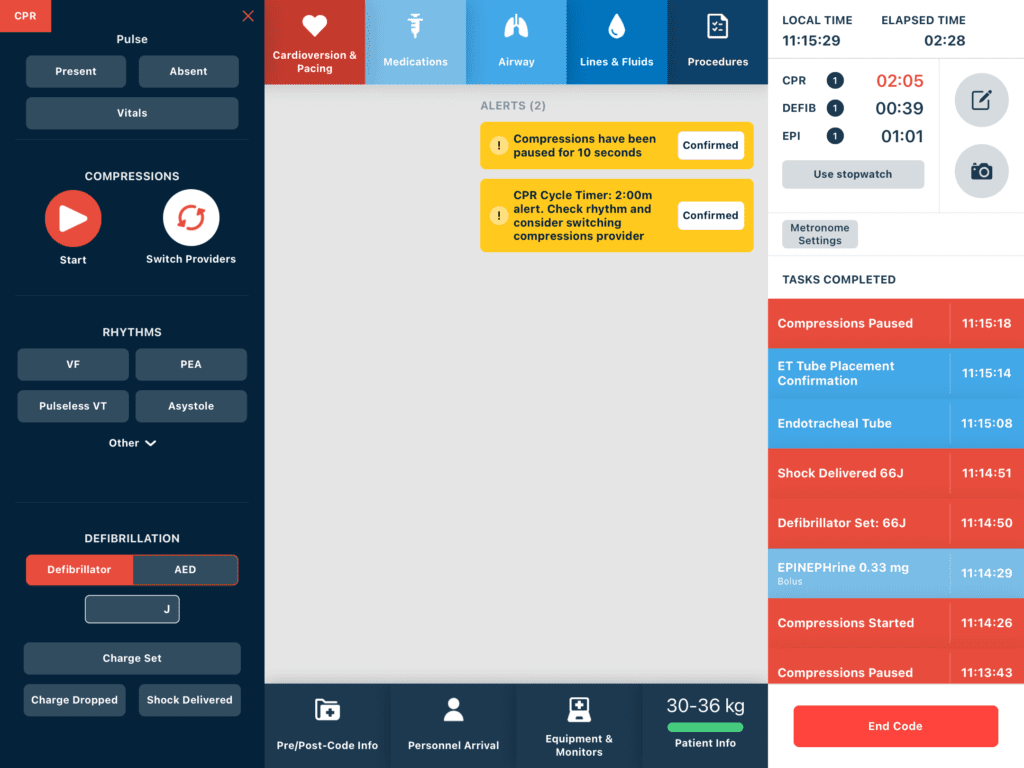
The timing of every medication, every procedure, and, in fact, every patient care intervention becomes critical to improving patient outcomes. The American Heart Association (AHA) has recognized the importance of careful timing of many of the life-saving cardiac arrest interventions, such that, a number of their published practice guidelines are based on very careful timing of their execution.
The process of recording and tracking each management decision that includes monitoring each event and time, as well as documenting these events and interventions according to National Standards is a daunting task. Not only does the recorder now need to accurately capture the events of the Code Blue, but now they are also tasked with tracking multiple timed and recurrent critical medication and management actions. This role is further complicated by the recorder having to “watch the clock” at the same time that they are trying to capture each event.
The Event
During a cardiac arrest, Guidelines², in part, suggest that:
- Epinephrine should be delivered at 3-5 minute intervals.
- Chest compressions must be delivered at a rate of 100-120 per minute.
- The person providing compressions should be rotated every two minutes to ensure that the compressor does not fatigue and the patient continues to receive adequate CPR.
- Compressions are paused every 2 minutes to take vitals, administer defibrillatory shocks, facilitate endotracheal intubation when managing patients with difficult airways, but compressions should never be paused for longer than 10 seconds.
- Defibrillation shocks should be delivered every 2 minutes.
Unfortunately, a Code Blue care recorder is frequently unable to track all of these time-based interventions during a fast-paced and high-stress resuscitation. How does one keep one’s eye on multiple clocks and at the same time generate an accurate Code Blue record?
In response to this dilemma, some hospital systems have begun deploying two recorders to code blues – one to actually document the event for the patient record and another to keep track of the timing. This presents a number of challenges, including overcrowding in the resuscitation space, taking an additional member away from other patient care duties and both “recorders” are prohibited from performing other duties related to resuscitation.
In addition, an active resuscitation scene presents a number of distractions. It is strongly suggested that the recorder do nothing but document the event.
Fortunately, a new Code Blue recording system has recently come on the scene to help alleviate the timing troubles and manual errors inherent in paper recording – RevitalPro – an intuitive, mobile, easy to use tablet-based device.

This system is the best Code Blue documentation system currently on the market. The system provides the Code Blue recorder with an interface that is exceptionally intuitive, easily used, designed around the workflow of a Code Blue. The system’s interface was designed with the user in mind. It requires little initial training or regular in-service training. In addition, the system provides automatic critical timers and safety alerts based on established guidelines. The timers and alerts have eliminated the need for the recorder to watch the clock or a stopwatch, and thus, concentrate exclusively on capturing the most complete, detailed, accurate patient record possible.

Brian Ross, PhD, MD
Professor Emeritus, Department of Anesthesiology and Pain Medicine, University of Washington
